Mercredi, 26 novembre 2025
|
09:00 – 09:30
|
Enregistrement |
|
|
Break
|
||
|
09:30 – 10:30
|
Conférence principale 1De l’évidence à l’empathie : approches mondiales en soins palliatifs |
|
|
Salle de concert
Conférence principale
|
David Blum, Zürich
|
|
La compassion : est-ce vraiment utile ?
Philipp Larkin, Lausanne
|
||
Less is More: Achieving Big Results with Limited Resources in Palliative Care
Christian Ntizimira, Kigali, Rwanda, Africa
|
||
|
10:30 – 10:50
|
Pause café |
|
|
Break
|
||
|
10:50 – 11:00
|
Mot de bienvenue |
|
|
Salle de concert
Special Session
|
||
par palliative.ch
Manuela Weichelt, Präsidentin palliative.ch
|
||
|
11:00 – 11:45
|
Conférence principale 2L’être humain au centre |
|
|
Salle de concert
Conférence principale
|
Sandra Eckstein, Basel
|
|
Einführung
Sandra Eckstein, Basel
|
||
Mensch sein - Mensch bleiben: zwischen Spitzenmedizin und Würde am Lebensende
Sandra Eckstein, Basel
|
||
|
11:45 – 12:00
|
Temps de transition |
|
|
Break
|
||
|
12:00 – 13:00
|
Séminaire parallèle 1 |
|
|
Salle de concert
Séminaire
|
Tanja Fusi-Schmidhauser, Lugano
|
|
|
FM1
Referral criteria of high-grade glioma patients to palliative care
Caroline Hertler, Zürich
AbstractHintergrund Patients suffering from high grade glioma, the most aggressive malignant primary brain tumor, have a very limited life span of 12-14 months. More importantly, they often suffer from early onset neurocognitive deficits and communication impairment, directly impacting the capacity to express their wishes and expectations for advanced care planning. Therefore, early integration of advanced care planning and supportive care must take place early. Ziel Here, we aim at characterizing factors triggers and barriers to referral of glioma patients to the outpatient palliative care consultation service, and to assess the main needs expressed by the patients. Methode In this retrospective study, we analyzed 91patients with glioma treated in the outpatient clinic of the Comprehensive Cancer Center Zurich between 2015 and 2024. We investigated demographics including clinical information, symptom burden, tumor information and support system implementation in the analyzed group. We also report on time frames of referral and survival. Statistical analysis was performed using SPSS Version 30. Resultate Patients with glioblastoma referred to our outpatient clinic had a mean age of 59.9 years (range 22-87) at first contact, of which 41.8% (n=38) women. Time from diagnosis to referral was 20.6 months in median and time from consultation to death was 5.1 months in median. More than 2/3 of patients first presented after the 3rd course of tumor-targeted treatment (73.6%, n=67) and showed recent clinical deterioration (79.1%, n=72) and progression in the imaging studies (81.3%, n=74) before consultation. A total of 7.7% (n=7) was no longer judicious at the time of consultation. Main reasons for referral were neurological and neurocognitive deterioration in 39.6% (n=36) patients, psycho-emotional patient burden in 18.7% (n=17) and patient wish in 13.2% (n=12). While caregiver burden was never a primaryreferral reason, we confirmed that 87.9% (n=80) of caregivers indicated burden symptoms. Schlussfolgerung While we found that glioma patients were referred to palliative care consultations earlier than the standard outpatient palliative population, they still presented mainly after failure of the last course of treatment, and with a very high symptom burden. Caregiver burden was a very frequent but underdiagnosed problem before referral. |
||
|
FM2
Training in Advance Care Planning conversations: A Structured Approach using the CORE framework
Sibylle Felber, Bern
AbstractHintergrund Advance Care Planning (ACP) discussions are essential for ensuring care aligns with patients’ values and goals. To ensure goal-concordant care, high-quality communication is central. A trusting, therapeutic relationship fosters this communication, enabling collaborative and person-centred care. To support clinicians in initiating and guiding meaningful ACP conversations, we developed a training program based on evidence-based components of relationship-centred care. Ziel The goal was to provide an easy to remember but effective framework to support clinicians in conducting state-of-the-art ACP conversations. This framework was then used to develop a one hour training programme for interprofessional oncology specialists for use in clinical practice. Methode The so-called ‘CORE’ framework is based on the quality communication principles from the Glasgow Consensus Statement (2024), following the Experiential Learning Cycle (Kolb 1984), and consists of the following components: Connect, Oberserve & Understand, Respond and Engage. On a content level, these components feed into to the prior developed iplan tool (www.iplan-care.ch) consisting of four steps: Prognosis, Life quality, Action Plan and Network. A one hour interprofessional training session was designed to train clinicians in conducting meaningful ACP discussions within a University Cancer Centre. Resultate This training was tested in two pilot sessions with each 6-8 oncology clinicians (specialist doctors and nurses). In semi-structured qualitative feedback from the participants, the sessions were perceived in terms of time as feasible as well as useful for clinical practice both in terms of content (CORE framework and iplan tool) and educational strategy (interactive teaching method). Schlussfolgerung CORE seems to offer an easy to use framework for clinicians guiding ACP discussions in daily practice. As part of a large-scale quality project, which aims to promote concurrent and goal-concordant care, the next step is to expand the ACP training to all clinicians working in the University Cancer Centre. |
||
|
FM3
«Ich kann das!» High Fidelity Simulation zur Selbstwirksamkeits-Förderung in der palliativen Pflege
Sara Häusermann, Winterthur
Abstract
Hintergrund
Palliative Care und damit verbunden auch familienzentrierte Pflege sind zentrale Themen der Pflegepraxis und -ausbildung. Studien zeigen, dass die Selbstwirksamkeit von Bachelor Pflege-Studierenden durch High Fidelity Simulation gestärkt werden kann.
Ziel Ziel der Studie war es, den Mehrwert von High Fidelity Simulation in Kombination mit traditionellen Lernmethoden bzgl. Entwicklung der Selbstwirksamkeit von Bachelor Pflege-Studierenden in einer familienzentrierten, frühen palliativen Pflegesituation bei hospitalisierten Erwachsenen zu explorieren. Methode Es wurde eine konvergente Mixed Methods-Studie durchgeführt. Im quantitativen Studienstrang (quasi-experimentell, repeated measures) wurde die Selbstwirksamkeit mit der Family Nursing Practice Scale (FNPS) bzw. der Selbstwirksamkeits-Subskala des Bonner Palliativwissenstest (BPW) zu vier Zeitpunkten (t1 = vor den Theorie-Modulen; t2 = nach den Theorie-Modulen; t3 = unmittelbar nach der High Fidelity Simulation; t4 = 3 Monate nach der High Fidelity Simulation) gemessen. Die quantitativen Ergebnisse wurden zusammen mit den in Fokusgruppen-Interviews erhobenen, durch eine qualitative Inhaltsanalyse generierten qualitativen Ergebnisse in ein Joint-Display eingefügt und Mixed Methods Meta-Inferenzen generiert. Resultate Im quantitativen Studienstrang nahmen 46, im qualitativen 22 Studierende teil. Im quantitativen Studienstrang ergaben sich keine Hinweise gegen die Modellannahmen. Zudem zeigten sich statistisch signifikante Differenzen bezüglich FNPS zwischen t1 und t3 (p = ,0019) sowie zwischen t1 und t4 (p = ,0198), und bezüglich BPW zwischen t1 und t3 (p <,0001), t1 und t4 (p = ,0012) sowie t2 und t3 (p = ,0112). In den Mixed Methods Meta-Inferenzen zeigte sich der Mehrwert der High Fidelity Simulation durch die Möglichkeit von Reflexion, Synthese und insbesondere durch die Wichtigkeit der praktischen Studierenden-Erfahrung, die Familie ins Symptommanagement einzubeziehen. Schlussfolgerung Die High Fidelity Simulation in Kombination mit traditionellen Lernmethoden kann einen Mehrwert bzgl. Entwicklung der Selbstwirksamkeit von Bachelor Pflege-Studierenden haben und sie in ihrer zukünftigen Rolle als Pflegefachpersonen bezüglich familienzentrierter Pflege und früher Palliative Care bei hospitalisierten Erwachsenen stärken. |
||
|
FM4
In der Praxis bewährt: Nachhaltige PROMs-Implementierung in der Palliativversorgung im Akutspital
Christa Hauswirth Siegenthaler, Winterthur
AbstractHintergrund Mit patientenberichteten Ergebnismessinstrumenten (PROMs) können Behandlungsergebnisse systematisch erfasst werden. Ziel Diese PROMs Daten können zur Qualitätsverbesserung der Palliativversorgung eingesetzt werden. Methode Das Zentrum für Palliative Care (ZfPC) am Kantonsspital Winterthur setzt seit vier Jahren PROMs (Adaptierte-Australische Karnofsky Performance Status (AKPS), Integrated Palliative Care Outcome Scale (IPOS) und Palliativphase) systematisch auf der Bettenstation ein. Die Palliativphase wird täglich eingeschätzt und im elektronischen Dokumentationssystem festgehalten; AKPS und IPOS werden bei Eintritt, Palliativphasenwechsel und Austritt/Tod der Patient:innen gemessen. Die Implementierung, welche sich am Consolidated Framework for Implementation Research (CFIR) orientierte, wurde intern von einem klinischen Champion, wöchentlich auch von einem Quality Improvement Facilitator begleitet. Resultate Nach initialer und fortlaufender Schulung aller Pflegefachpersonen und Ärzt:innen, wurden PROMs systematisch bei allen in das Projekt eingeschlossenen Patient:innen (n=1'282, n=1'486 Fälle) in einem Zeitraum von über vier Jahren erfasst. Der Grossteil (30%) der Patient:innen waren zwischen 70-79 Jahre alt. Die meisten Patient:innen (60%) sind an einem Tumorleiden erkrankt. Die IPOS Symptome Familienangst, Fatigue, eingeschränkte Mobilität, Angst, Depression und Schmerzen waren die meistbeobachteten Symptome bei Eintritt. Nach einer durchschnittlicher Liegedauer von 9.2 Tagen (SD 6.6 Tage) traten im Längsschnitt deutliche Verbesserungen bei Austritt oder Tod in der Prävalenz von den mässig bis sehr stark ausgeprägten IPOS Symptomen Schmerzen, Fatigue, Appetitlosigkeit, Verstopfung, Eingeschränkte Mobilität sowie Angst/Sorge der Patient:innen und Praktische Probleme auf. IPOS Symptome Atemnot, Mundtrockenheit, Familienangst, Nicht im Frieden mit sich selbst sein, Gefühle teilen und Informationsbedürfnisse zeigten einen geringfügigeren Rückgang in der Prävalenz bei Austritt oder Tod. Die Prävalenz bei Austritt oder Tod war für kein IPOS Symptom höher als bei Eintritt. Patient:innen, welche in der instabilen Phase eingetreten sind, waren bei Austritt überwiegend in der stabilen Palliativphase. Schlussfolgerung Am ZfPC gelang die erfolgreiche und nachhaltige Einführung von PROMs. Die erhobenen Daten erlauben Rückschlüsse auf die Wirksamkeit und Qualität der erbrachten Versorgung und sind eine wertvolle Grundlage für die Qualitätsentwicklung. |
||
|
12:00 – 13:00
|
Séminaire parallèle 2 |
|
|
Salle des sociétés
Séminaire
|
David Blum, Zürich
|
|
|
FM6
Emotions and Self-Disclosure in Serious Illness Conversations: Effects on Trust, Compassion, and Professionalism
Robert Staeck, Bern
Abstract
Hintergrund
Physicians are often reluctant to express emotions or share personal experiences with patients due to concerns about appearing unprofessional or crossing boundaries. However, research on perceptions of these behaviors remains limited. Ziel We examined how personal and emotional self-disclosure by physicians shapes perceptions of compassion, trust, professionalism, and comfort in the context of a serious illness consultation. Methode We conducted a factorial vignette study with 1,572 participants from the Swiss general public (51.4% women), each of whom rated 5 vignettes. Each vignette systematically varied eleven aspects of the consultation, including whether the physician disclosed a personal experience, showed sadness (with or without tears), or the clarity of their communication. Participants rated each vignette on compassion, trust, professionalism, and comfort using 11-point scales. We analyzed the data using multilevel regression models with random intercepts. Resultate Clarity of information and longer consultations were the strongest positive predictors across all outcomes. Expressions of sadness, especially when accompanied by visible emotion, and personal self-disclosure were also significantly associated with higher ratings of compassion, trust, and comfort, with no evidence of negative effects on ratings of professionalism. The combination of self-disclosure and emotional expression consistently led to the highest scores for all outcomes, except for compassion, where emotional expression without self-disclosure achieved similar gains as strong as the full combination. Schlussfolgerung Physician self-disclosure and emotional expression consistently enhanced compassion, trust, and comfort ratings and did not diminish perceived professionalism. Our findings challenge common assumptions in medical culture and suggest these behaviors have a strong potential to support relationship-building even under constrained conditions. |
||
|
FM7
Das macht den Unterschied: Kosten von spezialisierter Palliative Care im Universitätsspital
Maud Maessen, Bern
AbstractHintergrund Die Literatur hebt die Vorteile spezialisierter Palliative Care (sPC) zur Verbesserung der Versorgungsqualität am Lebensende hervor. Studien zu den ökonomischen Aspekten der Palliativversorgung sind jedoch rar, besonders in Europa. Laut OECD belasten die letzten Lebensmonate – insbesondere durch Spitalkosten – die Gesundheitssysteme stark. Dabei bleibt oft unklar, wofür genau die Mittel verwendet werden. Vorliegende, meist US-amerikanische, Kostenanalysen liefern uneinheitliche Ergebnisse und betrachten selten einzelne Kostenarten wie Medikamente, Verbrauchsmaterialien, Labordiagnostik, Unterkunft, Verpflegung, ärztliche Leistungen, Pflege, therapeutische Massnahmen oder soziale Beratung differenziert. Ziel Diese Studie vergleicht unterschiedliche Kostenarten bei verstorbenen Patient:innen eines Universitätsspitals, mit sPC und ohne palliativmedizinische Intervention (usual care, UC). Methode Analysiert wurden retrospektiv medizinische und administrative Spitaldaten von 4'316 Patient:innen, die zwischen Januar 2016 und Dezember 2022 in einem Universitätsspital verstorben sind. Die Kosten wurden mithilfe von inverse probability weighting auf Basis von Propensity Scores adjustiert. Resultate Die durchschnittlichen täglichen Behandlungskosten fielen in der Gruppe mit sPC mit CHF 2'607 niedriger aus als in der UC-Gruppe, bei der durchschnittlich CHF 3'007 pro Tag anfielen. Dennoch lagen die Gesamtkosten des Spitalaufenthalts in der sPC-Gruppe mit CHF 31'350 über jenen der UC-Gruppe (CHF 20'321), was primär auf längere Verweildauern in der sPC-Gruppe zurückzuführen ist. Die Zusammensetzung der Kosten pro Tag unterschied sich zwischen den Gruppen deutlich: Während sPC-Patient:innen höhere Ausgaben für pflegerische Leistungen und therapeutische Massnahmen verursachten, entfielen bei UC-Patient:innen höhere Kosten auf diagnosebezogene Leistungen wie Laboruntersuchungen, Medikation, Verbrauchsmaterialien und ärztlich geleitete Interventionen. Bemerkenswert ist, dass Patient:innen, die innerhalb der ersten drei Spitaltage eine sPC-Intervention erhielten, deutlich niedrigere Gesamtkosten aufwiesen als Patient:innen ohne frühzeitige sPC-Versorgung (CHF 22'999 vs. CHF 60'691; p < 0.001). Schlussfolgerung Unsere Ergebnisse bestätigen: sPC macht einen Unterschied. Am Lebensende zeigte sich in der sPC-Gruppe eine unterschiedliche Kostenstruktur – mit mehr Interaktion und weniger Intervention. |
||
|
FM8
Estimating the Prevalence and Cost of Life-limiting Conditions in Children in Switzerland
Hans-Ulrich Bender, Bern
Abstract
Hintergrund
Palliative care for children in Switzerland is structurally underdeveloped. The Federal Office of Public Health funded this study in order to understand the demand for such services at any given time. Previous studies using catalogues of life-limiting conditions (LLC) have indicated a rising prevalence of affected children, yet with notable variation in numbers. Ziel This study estimates the prevalence and the cost of LLC in children in Switzerland to aid in planning future palliative care services. Methode We retrospectively analysed hospital data using an ICD-10 catalogue of LLC developed by Fraser et al. (2021) for the United Kingdom (UK). In a first pilot study, we analysed data from four university hospitals and one regional hospital covering five years (2018-2022) and five cantons. In a second step, we analysed national hospital data and financial data provided by the Federal Statistics Office covering ten years (2013-2023) using the same catalogue. Resultate The prevalence of LLC in children in our first study increased from 30.9/10,000 in 2018 to 37.9/10,000 in 2022, equivalent to ~6600 children with a LLC in Switzerland in 2022. In the second study, the prevalence increased from 28.0/10’000 in 2013 to 36.8/10’000 in 2023 confirming our first results. Prevalence is highest and rising the most in children aged < 1 year (236.7/10’000 in 2013 to 472.6/10’000 children in 2023). Congenital anomalies, perinatal and neurological conditions were the most prevalent diagnoses in both datasets depending on age group. The median hospital cost per patient with a LLC increased by 19.8% (2013-2023). In relation to the gross domestic product (GDP), the total hospital cost for these children increased by 37.8% accounting for 0.43% of the entire healthcare spending in 2023. Schlussfolgerung This is the first study estimating the prevalence of LLC in Switzerland and it confirms a rising prevalence, particularly among very young children. It highlights the need for prioritized development of paediatric palliative care services in this group emphasizing that these services should be a genuinely paediatric domain. At the same time, we show that median hospital healthcare expenditure per patient rose by only half as much as total spending for children with LLC. Additionally, this group accounted for less than 0.5% of total healthcare expenditure in 2023 relative to the GDP. |
||
|
12:00 – 13:00
|
Séminaire parallèle 3 |
|
|
Salle d'atelier 5
Séminaire
|
Gora Da Rocha Rodrigues, Lausanne
ContexteLa réflexivité est une compétence clé en recherche, particulièrement lorsqu’il s’agit de thèmes sensibles tels que la mort, le mourir et la souffrance. Si la réflexivité est souvent associée à l’analyse des données, elle joue un rôle tout aussi essentiel dans les premières étapes de la recherche : conception, collecte et interactions sur le terrain. En soins palliatifs, le caractère émotionnel et imprévisible du terrain peut fragiliser les chercheur-e-s, souvent dépourvus de soutien structuré pour réfléchir à leurs pratiques et à leurs vécus. Objectif Afin de répondre à ce besoin, un Laboratoire de Réflexivité a été créé en août 2023 au sein du service de soins palliatifs d’un hôpital universitaire suisse. Inspiré du modèle proposé par la sociologue Hella von Unger, ce dispositif vise à renforcer la réflexivité des chercheur-e-s — cliniques et non cliniques — impliqués dans des terrains liés à la fin de vie. Le Laboratoire offre un espace sécurisé pour partager des expériences, explorer des dilemmes et réfléchir collectivement aux enjeux méthodologiques, éthiques et émotionnels du travail de terrain. Description Les rencontres ont lieu chaque mois, en français ou en anglais, en présentiel ou à distance. Les participant-e-s, issu-e-s de disciplines diverses (médecine, soins infirmiers, sociologie, anthropologie, linguistique, psychologie), mènent leurs recherches dans différents contextes en Suisse. Chaque année, un thème commun est choisi et exploré à travers des discussions, des projets collaboratifs et des exercices autoethnographiques. Résultats Le Laboratoire de Réflexivité contribue à améliorer le bien-être des chercheur-e-s, à renforcer la collaboration interdisciplinaire et à enrichir la qualité scientifique des travaux. Depuis sa création, il a donné lieu à deux publications et à plusieurs communications, notamment sur les interactions chercheur–patient en soins palliatifs (2024) et sur le rôle des intermédiaires de recherche (2025). |
|
|
FM9
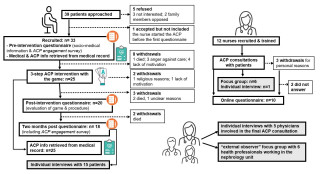
Advance Care Planning in Dialysis Patients with Anticip’action: quantitative acceptability study
Christine Clavien, Genève
AbstractContexte To support advance care planning (ACP), a conversation game – Anticip'action – and a connected 3-step ACP intervention using the game were developed. Objectiv This study assesses the acceptability, feasibility and effect of the intervention with patients undergoing dialysis at a tertiary hospital. Méthode Dialysis nurses received a 10-hour training in ACP and use of the card game Anticip’Action. All patients dialysed in the division of nephrology were eligible. Acceptability and feasibility were assessed with questionnaires and note taking. Effect was assessed with pre-post number of advance directives (AD), number of patients designating a surrogate, quality of written ACP documentation, patients’ responses to the 9-items ACP Engagement Survey, and patients’ assessment of their ACP documentation. Résultats 12 nurses conducted ACP interventions. 33 patients (87% of eligible patients) accepted to be included, 25 (75%) started the ACP intervention, 23 completed it, and 18 answered all questionnaires. 5 withdrawals were due to premature death. Nurses and patients rated the training, the intervention and the card game as good and highly acceptable: mean scores ranged from 2.87 to 4.17 on 5-point Likert scale questions. Organizational difficulties were reported by nurses. Significant increases were observed on uploaded AD (+30%), designated healthcare surrogates (+80%), patients reporting end-of-life planning actions (12/19), patients’ engagement in ACP (+1.04 on 1-5 scale, p= <.001), quality of ACP documentation (+2.68 on a 1-5 scale, p= <.001), and patients’ evaluation of their ACP documentation (3.44 ±1.04 on 1-5 scale). Conclusion The 3-step ACP intervention using Anticip’action showed good implementation potential in clinical context. 
|
||
|
FM10
Negotiating legitimacy in making ‘reasonable’ decisions for people lacking decision making capacity
Laura Jones, Lausanne
AbstractContexte When residential aged care facility (RACF) residents lose medical decision-making capacity, their health care proxies are called upon to make medical decisions. Anticipatory models, such as advance care planning (ACP) by proxy, aim to make anticipatory orders in case of medical emergency on behalf of residents. This process involves health care proxies, physicians and ACP facilitators discussing the most appropriate course of action in case of emergency. Objectiv To explore the rhetoric devices and interpretive repertoires employed by health professioanals and health care proxies when establishing their legitimacy to make 'reasonable' decisions on behalf of a person lacking medical decision making. Méthode We audio-recorded 15 naturalistic ACP by proxy discussions and conducted a discourse analysis to identify the discursive devices and rhetorical strategies used to legitimise actor’s authority in anticipatory decision making on behalf of a person who no longer has medical decision-making capacity. Résultats Health care proxies, ACP facilitators and physicians deploy a range of discursive devices to legitimise their claims as to what constitutes ‘reasonable’ treatment for a person who has lost medical decision-making capacity. Health care proxies drew on their next of kin relationship, lifespan knowledge of the person, their previous and current implication in the person’s life, their closeness and their knowledge of the person’s medical history. Physicians draw on notions of the trajectory of the person’s illness/conditions, their observations of other ‘similar’ people and their medical expertise. RACF ACP facilitators draw upon their current day-to-day knowledge of the person, their experience with other RACF residents and their medical knowledge. Such constructs are deployed to co-construct an agreed upon plan for future action in case of an emergency situation, however, when opinions of ‘reasonable’ action differ, the territories of ‘closeness’ and ‘medical knowledge’ are contested. Here, we present this contested territory. Conclusion Analysing the ways in which actors involved in planning future treatment for people lacking medical decision-making capacity sheds light on the multiple perspectives and difficulties being attended to in such discussions, and provides insights for care planning for a growing population. |
||
|
FM11
Between Needs and Barriers: Integrating Palliative Care into the Trajectory of Advanced Respiratory Diseases
Lisa Hentsch, Genève
AbstractContexte Patients with progressive respiratory diseases experience debilitating physical and psychological symptoms that worsen as the disease advances. It is well established that their access to palliative care (PC) remains limited and often occurs at a late stage, sometimes at the very end of life. Objectiv The aim of this study is to explore how to integrate PC earlier and more appropriately into the management of these patients. Méthode A qualitative study using focus groups (FG) was conducted with a purposive sample of patients with chronic respiratory diseases (stage 3 or 4 COPD according to GOLD, or advanced fibrotic interstitial lung disease) and their informal caregivers. Data were analyzed by two independent researchers using Braun and Clarke’s thematic analysis method, supported by the MAXQDA software. Résultats A total of 5 patients and 5 informal caregivers participated in two separate focus groups, each lasting an average of 83 minutes. The term "palliative care" raised questions and concerns. Participants emphasized the need to clarify the goals of palliative care, highlighting the importance of preserving quality of life. They advocated for the systematic introduction of PC from the time of diagnosis, outside of crisis situations. Group discussions, such as roundtables during pulmonary rehabilitation, were identified as effective ways to introduce PC, especially by benefiting from peer experiences. Participants agreed that discussions about care planning and advance directives not only reduce the decision-making burden on caregivers but also reassure patients by ensuring their wishes will be respected. Table 1 presents a summary of the main themes. Conclusion After receiving information about the goals of palliative care, patients clearly expressed a desire to access it early in order to better manage symptoms, receive continuous support, and anticipate future care. Table 1 – How to Introduce Palliative Care Early and Appropriately – Main Themes 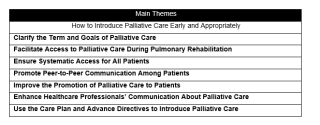
|
||
|
FM12
Un Laboratoire de Réflexivité dans un service de soins palliatifs : innover la recherche de l’intérieur
Anca-Cristina Sterie, Lausanne
AbstractContexte La réflexivité est une compétence clé en recherche, particulièrement lorsqu’il s’agit de thèmes sensibles tels que la mort, le mourir et la souffrance. Si la réflexivité est souvent associée à l’analyse des données, elle joue un rôle tout aussi essentiel dans les premières étapes de la recherche : conception, collecte et interactions sur le terrain. En soins palliatifs, le caractère émotionnel et imprévisible du terrain peut fragiliser les chercheur-e-s, souvent dépourvus de soutien structuré pour réfléchir à leurs pratiques et à leurs vécus. Objectif Afin de répondre à ce besoin, un Laboratoire de Réflexivité a été créé en août 2023 au sein du service de soins palliatifs d’un hôpital universitaire suisse. Inspiré du modèle proposé par la sociologue Hella von Unger, ce dispositif vise à renforcer la réflexivité des chercheur-e-s — cliniques et non cliniques — impliqués dans des terrains liés à la fin de vie. Le Laboratoire offre un espace sécurisé pour partager des expériences, explorer des dilemmes et réfléchir collectivement aux enjeux méthodologiques, éthiques et émotionnels du travail de terrain. Description Les rencontres ont lieu chaque mois, en français ou en anglais, en présentiel ou à distance. Les participant-e-s, issu-e-s de disciplines diverses (médecine, soins infirmiers, sociologie, anthropologie, linguistique, psychologie), mènent leurs recherches dans différents contextes en Suisse. Chaque année, un thème commun est choisi et exploré à travers des discussions, des projets collaboratifs et des exercices autoethnographiques. Résultats Le Laboratoire de Réflexivité contribue à améliorer le bien-être des chercheur-e-s, à renforcer la collaboration interdisciplinaire et à enrichir la qualité scientifique des travaux. Depuis sa création, il a donné lieu à deux publications et à plusieurs communications, notamment sur les interactions chercheur–patient en soins palliatifs (2024) et sur le rôle des intermédiaires de recherche (2025). |
||
|
12:00 – 13:00
|
Séminaire parallèle 4 |
|
|
Salle d'atelier 1+2
Séminaire
|
Mathieu Bernard, Lausanne
|
|
|
FM13
Prosociality from patients towards healthcare professionals: another way to be part of and depart
Fanny Bovey, CHUV, Lausanne
Abstract
Contexte
Prosociality, defined as an action designed to benefit others, is a desire that can be very present at the end of life, despite physical and psychological vulnerability. Scientific literature shows that this tendency increases with lowering life expectancy, and that being able to express prosociality may contribute to lower levels of depression and anxiety. Recognizing patients’ needs and capacity to be prosocial goes beyond patient-centered care, as it requires their recognition as partners and providers, genuinely interested in benefiting others and not only their own care. This recognition is particularly important in contexts of asymmetry (carer / cared for), as it allows patients to maintain a sense of dignity and purpose. Objectiv We examine how patients express prosociality in daily interactions with health practitioners, in palliative care. Our aim is to highlight the forms that patients’ prosociality takes in interactions. Méthode We collected 87 video recordings of interactions between 8 patients and 47 HPs in two palliative care units in French-Speaking Switzerland. Extracts in which patients display prosociality were transcribed and analyzed, using thematic analysis (to examine content) and conversation analysis (to examine in situ organization of verbal and non-verbal communication). Résultats We identified 5 forms of prosociality : 1. Gratitude, as an expressed recognition for HPs' work; 2. Compliments and concerns for HPs, about their work but also their life out of the hospital; 3. Help in care (e.g. to help with manoeuvres; collection of informations on their health; passing on of their expertise while respecting that of HPs); 4. Alleviate dying's stigma (e.g. to anticipate talks on decay and death, talk about it using humor, minimize their problems); 5. Trust, expressed deliberately as giving ("I'm in your hands"), to confirm relationships and take an active role in letting go. Conclusion The fact that patients initiate and display prosociality under so diverse formats underlines their autonomy, wish and claim to be considered both as partners and providers, playing an active role in their dying process. It is thus a way to escape the asymmetry of the care relationship, that can often be overbearing in medical contexts. Considering and understanding prosociality helps considering patients in palliative care as a whole. Our focus on interactions shows how prosociality is organized in situ, in ordinary, sometimes “banal” interactions. Analysing these situations can give tools to professionals to help noticing these instances, recognize and support patients to express themselves. |
||
|
FM14
Soins palliatifs intégrés en gériatrie aiguë hospitalière: une étude de mise en œuvre
Sandra Rastrelli, Locarno
Abstract
Contexte
Le vieillissement de la population entraîne une augmentation de la demande en soins palliatifs (SP) et gériatriques. Les unités de gériatrie aiguë accueillent des patients fragiles présentant des symptômes complexes tels que la dyspnée, la douleur, l’asthénie, les crises existentielles – des problématiques centrales pour les deux disciplines. L’objectif partagé entre la gériatrie et les SP est d’améliorer la qualité de vie, d’atténuer la souffrance et de respecter la dignité du patient. Malgré les bénéfices documentés de l’intégration des SP en gériatrie, de nombreux patients âgés n’ont pas accès à ces services et des obstacles persistent dans la collaboration entre les deux secteurs. Objectiv Cette étude vise à intégrer les SP dans le cadre de la gériatrie aiguë, en assurant une prise en charge précoce. Les objectifs principaux incluent: l’activation rapide de l’équipe de SP, la planification anticipée des soins, le contrôle symptomatique dans les 48 heures et l’implication des proches/aidants dans le parcours de soins. Méthode L'étude comprend une analyse des dossiers médicaux des patients admis en gériatrie aiguë à l'aide de l'outil ID-PALL©, la conduite de focus group et d'entretiens interprofessionnels semi-structurés afin d'explorer les ressources et les difficultés. Un groupe de travail a défini les stratégies de mise en œuvre qui comprennent : des sessions de formation sur l'utilisation d'ID-PALL© et les principes des SP, le remplissage d'ID-PALL© pour tous les patients admis et l'orientation automatique vers les SP au cours d'une phase de test de deux mois. Ensuite, l'étude de prévalence et les groupes d'évaluation seront répétés. Résultats Pendant un peu plus de la moitié de la phase de test, le nombre d'annonces de SP a presque égalé le nombre enregistré pour l'ensemble de l'année 2024. Sur les 25 évaluations soumises jusqu'au 20 mai 2025, 23 ont confirmé l'identification correcte des patients spécialisés en SP. Les professionnels impliqués rapportent une amélioration significative de la collaboration avec une intégration plus fluide entre les deux spécialités. Conclusion Les résultats préliminaires suggèrent que l’objectif est en voie d’être atteint. L’étude démontre qu’il est possible d’améliorer l’accès des patients âgés aux SP grâce à une approche structurée et multidisciplinaire. Des études futures pourraient explorer l’impact à long terme de cette collaboration sur la qualité de vie des patients et sur l’évolution des pratiques cliniques en gériatrie. |
||
|
FM15
Barriers and facilitators to Advance Care Planning by proxy in Swiss nursing homes
Samira Ruedin, Lausanne
Abstract
Contexte
Advance Care Planning promotes care that is coherent with patient wishes in the event that they lose decision-making capacity (DMC). However, many people lose DMC before participating in anticipatory care planning. For this situation, models of advance care planning by proxy (ACP by proxy), i.e. conducted with health care proxies, are under development. Objectiv We aimed to test the acceptability and feasibility of an ACP-bp model in Swiss Residential Aged Care Facilities (RACFs). Méthode Design: Single-arm pilot study of the acceptability and feasibility of an ACP by proxy intervention in Swiss RACFs (n=4). Data: Semi-structured interviews were conducted with ACP-bp facilitators pre (n=15) and post (n=6) intervention, as well as with health care proxies (n=21) post-intervention. Reflexive Thematic Analysis was employed to identify themes explaining the barriers and facilitators to conducting ACP-bp in this context. Résultats Acceptability of the intervention was high, with both health professionals and health care proxies reporting many benefits including improved communication between proxies, health professionals and physicians, deeper understanding of the residents as persons, and increased confidence in providing care that is coherent with resident wishes. Implementation of the intervention was promoted by having a health professional ‘champion’ ACP-bp, having a director who supported ACP-bp, flexibility in work structure that allowed ACP-bp, and a dedicated person for coordinating meetings. Implementation was hindered by RACF staff turnover, lack of health professional and health care proxy time, physicians who were not engaged, and health professional and health care proxy reluctant to engage in planning discussions. Conclusion ACP-bp is valued and helpful when implemented. Yet, implementation in the RACF setting is hindered by multiple factors predominantly related to the general RACF working context. Improvement of the systemic factors is necessary in order to promote ACP-bp and thereby respect autonomy of people who no longer have DMC. |
||
|
FM16
Unequal goodbyes: inequalities in end-of-life care before and after the pandemic across 28 countries
Paola Sillitti, lausanne
AbstractContexte The COVID-19 pandemic significantly disrupted health systems, impacting how individuals received end-of-life (EOL) care and amplifying pre-existing inequalities in healthcare access. While research has examined the burden placed on healthcare professionals, less attention has been paid to the experience of care recipients in their final year of life, particularly across different socioeconomic groups. Objectiv This study explores the sociodemographic factors associated to the type of care that people received before death before and after the outbreak of the pandemic across Europe. Méthode The analysis uses data from 5,029 deceased individuals aged 50 and older across 28 European countries, drawn from waves 7–9 (2018–2022) of the Survey of Health, Ageing and Retirement in Europe (SHARE). Information was collected via proxy interviews post-mortem and includes details on health, care received in the final year of life, and sociodemographic characteristics. The main outcomes were six binary variables indicating the receipt of hospital, hospice, nursing home, home care, care from a general practitioner (GP), and from a specialist physician. Using multinomial probit regression models, we estimated the average marginal effects of dying after the onset of the pandemic (March 2020), with interaction terms for cause of death, education level, and financial difficulty. Résultats Overall, EOL care access declined following the pandemic’s onset, with particularly steep reductions in home-based care and specialist services. These changes were uneven across population groups. Individuals who died from cardiovascular or infectious causes experienced significant declines in hospital, home, and specialist care. Socioeconomic disparities widened: decedents with low education experienced decreases across all care types except nursing homes, while individuals with financially hardships saw marked reductions, particularly in home care and specialist care. Conversely, those with higher education or financial security saw smaller or no significant changes. Cancer decedents experienced the most stable patterns of care. Conclusion The findings suggest that the pandemic exacerbated pre-existing inequalities in EOL care across Europe, disproportionately affecting those with lower education and financial resources. While institutional care remained relatively accessible for some, home and outpatient care saw significant declines, especially for vulnerable groups. These results underscore the urgent need for policies that build resilient, equitable EOL care systems capable of protecting disadvantaged populations in times of crisis. |
||
|
13:00 – 14:15
|
Buffet déjeuner & Présentation des posters |
|
|
Break
|
||
|
13:15 – 14:00
|
Symposium satellite |
|
|
Salle des sociétés
Symposium
|
||
Cannabis in der Palliativmedizin – Evidenz und Praxis
Thomas Herdegen, Kiel
Sponsor

|
||
|
13:15 – 14:00
|
Club littéraire Podcasts |
|
|
Salle d'atelier 1+2
Club littéraire
|
Monica Lonoce, Riehen
|
|
Kindern eine Stimme geben - Podcast Palli Pod
Gabriela Meissner, Urdorf ; Mercedes Ogal, Brunnen
|
||
Podcast « Toucher du doigt la santé »
Antoine Lacouturière, Peyrat le Château (F)
|
||
Capsule vidéo « Monique »
Natacha Madaule, Genève ; Muriel Delacquis, Genève ; Laurence Jelk Morales, Genève ; Anna Tahou, Genève
|
||
|
14:15 – 15:15
|
Club littéraire livres |
|
|
Salle d'atelier 1+2
Club littéraire
|
Gabriela Meissner, Urdorf
|
|
Schwellenzeiten – Wandelzeiten: Kraftvoll durch Lebenskrisen gehen
Sabrina Gundert, Alpnach Dorf
|
||
Sterben Gestalten
Julia Rehsamen, Bern ; Bitten Stetter, Zürich
|
||
Molina, die Trauerfee
Monica Lonoce, Riehen
|
||
Lebensbilder
Tina Ruisinger, Berlin (D)
|
||
|
14:15 – 15:15
|
Séminaire parallèle 5 |
|
|
Salle de concert
Séminaire
|
Eva Bergsträsser, Zürich
|
|
|
FM17
Lebensqualität ohne Psychopharmaka? – der vida cotidiana®-Ansatz für Menschen mit Demenz
Jana Andrina Lingenhel, Luzern
AbstractHintergrund Die steigende Lebenserwartung und die Zunahme chronischer Erkrankungen erhöhen den Betreuungsbedarf, besonders bei Menschen mit Demenz. In der Schweiz leben über 156’900 Demenzkranke, und diese Zahl wird aufgrund der alternden Bevölkerung weiter steigen, was den Bedarf an Betreuungsangeboten zur Sicherung der Lebensqualität und Wohlbefinden erhöht. Die Betreuung von Menschen mit Demenz ist besonders herausfordernd, da sowohl kognitive als auch behaviorale und psychische Symptome der Demenz (BPSD) spezialisierte Pflegekräfte und interdisziplinäre Zusammenarbeit erfordern und für Betreuende sowie Betroffene stark belastend sein können. Es gibt zunehmend Kritik an der Praxis, da Psychopharmaka häufig als erste Massnahme bei BPSD wie zum Beispiel Aggression in Betracht gezogen werden, obwohl häufig Neben- und Wechselwirkungen mit anderen Medikamenten auftreten und in vielen Fällen einfühlsame Betreuung und alternative Ansätze ebenso wirksam sein können. Diese Ansätze fördern das Wohlbefinden der Betroffenen und können herausforderndes Verhalten reduzieren, wodurch die Notwendigkeit für Medikamente verringert wird. Ziel Das entwickelte Demenzbetreuungskonzept vida cotidiana® setzt auf die Integration von Menschen mit neurokognitiver Beeinträchtigung, wie Demenz, in den Alltag. Durch natürliche Routinen, sinnvolle Aufgaben und die Erhaltung der Selbstwirksamkeit, soll die Würde und Lebensqualität der Betroffenen gesteigert werden. Dabei wird die Individualität der Menschen gewahrt und auf erzwungene Interventionen verzichtet. Ziel dieser Studie ist es, die Auswirkungen des Demenzbetreuungskonzepts vida cotidiana® auf die Lebensqualität, das Wohlbefinden und die Alltagsintegration von Menschen mit neurokognitiver Beeinträchtigung zu untersuchen. Methode Es wird eine retrospektive, longitudinale qualitative Studie mit fünf Bewohner:innen einer Institution durchgeführt, die das Demenzbetreuungskonzept vida cotidiana® umsetzt. Die Analyse umfasst eine Literaturübersicht, eine Inhaltsanalyse der Verlaufsdokumentationen und Medikamentenlisten sowie halbstrukturierte Interviews mit Angehörigen. Resultate Erste Erfahrungen aus der Institution zeigen, dass das Konzept die Lebensqualität der Bewohner:innen verbessert. Durch die qualitative Untersuchung sollen vertiefte Einblicke in die subjektiven Erfahrungen der Betroffenen und ihrer Angehörigen gewonnen und mögliche Wirkmechanismen des Konzepts identifiziert werden. Schlussfolgerung Erkenntnisse aus dieser Studie sollen genutzt werden, um eine umfassendere Untersuchung durchzuführen und den Einfluss des vida cotidiana®-Ansatzes auf Lebensqualität, Wohlbefinden und den Einsatz von Psychopharmaka wissenschaftlich fundiert zu aufzuzeigen. Zudem sollen die Ergebnisse als Grundlage für Handlungsempfehlungen und eine mögliche Implementierung in weiteren Einrichtungen dienen. |
||
|
FM18
"SOS in Moral Distress" - Ein Ethikmodell zur Verbindung von Autonomie, Best Interests und Shared Decision-Making
Jürg Streuli, Zürich
AbstractHintergrund In der Palliative Care stellen Entscheidungen unter Unsicherheit und mit existenziellen Konsequenzen eine besondere Herausforderung dar – insbesondere wenn Werte, Interessen und Sichtweisen zwischen Fachpersonen, Betroffenen und Angehörigen divergieren. Die Konzepte Autonomie, Best Interests und Shared Decision-Making (SDM) bieten wichtige Orientierung, bleiben aber in konflikthaften Situationen oft unzureichend. Ziel Vorstellung des Shared Optimum Schemas (SOS) als strukturierter Entscheidungsansatz zur ethischen Orientierung in komplexen Versorgungssituationen. Methode SOS wurde aus qualitativen Studien mit Fachpersonen und Familien entwickelt und in moderierten Teamprozessen in pädiatrischen und adulten Kontexten erprobt. Im Vortrag wird es anhand von exemplarischen Beispielsmoderationen vorgestellt. Die Moderation von SOS dauert in der Realität zwischen 60-90min. Der Prozess wird schematisch dargestellt. Resultate Anhand von drei Fallbeispielen – ein schwerkranker Säugling mit Eltern deine Therapieeskalation entgegen Empfehlung des Teams wünschen, ein 17-jähriger Jugendlicher mit Therapieverweigerung und eine ältere Person mit einem End-stage Lungenkarzinom und einer schwierigen Team-Familien-Interaktion – zeigt SOS, wie eine ethisch tragfähige Zone zwischen medizinischen, psychosozialen und normativen Grenzen entstehen kann. Diskussion SOS integriert bestehende Konzepte, betont jedoch klare Schadensschwellen, konkrete Autonomiefähigkeitn und eine dialogische Entscheidungsfindung als Prozess. Damit unterstützt es sowohl interprofessionelle Klarheit als auch die Einbindung von Betroffenen und Angehörigen. Schlussfolgerung SOS eignet sich insbesondere für ethisch anspruchsvolle Situationen über Altersgrenzen hinweg und bietet eine realistische, transparente und partizipative Alternative zu rein prinzipienbasierten Modellen oder eng gefassten Konzepten wie dem Best Interests Standard oder der Zone of Parental Discretion. 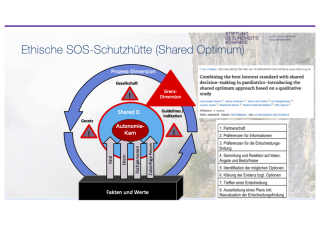
|
||
|
FM19
Sensorbasierte Belastungserfassung bei Patienten mit kognitiven Einschränkungen: Das Protokoll der SURREAL-Studie
Christopher Böhlke, Basel
AbstractHintergrund Given the well-documented sociodemographic shifts and the increasing prevalence of multimorbidity, the demand for palliative and end-of-life care is expected to increase significantly in the coming years. Digital health technologies have the potential to facilitate automated detection of distress in palliative care, including symptoms like pain, breathlessness (dyspnea), panic, agitation, and delirium. Such advancements could alleviate the suffering of cognitively impaired patients who are unable to call for help, for instance, by pressing an alarm button, yet urgently require professional intervention. Ziel This observational feasibility study aims to assess whether data output from a sensor system consisting of a 3-D-radar, photoplethysmographic sensors (wearables), and audio detection (microphones) is associated with patients’ distress events as identified by medical professionals during standard care. Methode We will utilize well-established sensor systems, including Qumea® and wearables, to monitor heart rate, respiratory rate, heart rate variability, body movements, postures, and audio signals, such as changes in sound intensity or voice frequency. Resultate Data will be compared against the current gold standard for detecting distress in cognitively impaired patients: assessments conducted by trained healthcare professionals, specifically specialist palliative care nurses and physicians. Schlussfolgerung Identifying correlations between sensor data and professional distress assessments could facilitate future validation studies, potentially leading to the development of automated distress detection systems using sensor arrays. |
||
|
FM20
“Cuidados paliativos desde la perspectiva pastoral”A Cooperation between Switzerland and Ecuador
Karin Tschanz, Brent
Abstract
Contexte
In Ecuador, according to the 2020 Atlas of Palliative Care in Latin America, the implementation of palliative care has seen significant progress. However, substantial challenges remain in achieving full coverage. Currently, the country has 4.6 palliative care teams per million inhabitants. With 78 teams, Ecuador occupies a mid-range position in the regional context. Objectiv One of the main barriers is limited access to information and training in palliative care for healthcare professionals, leading to widespread unawareness of palliative care. This lack of knowledge extends to families and caregivers as well. To address this, Swiss experts in palliative medicine and spiritual care organized a six-day, 40-hour course between September and October 2024. The goal was to share Swiss best practices across the four dimensions of palliative care (physical, psychological, social, and spiritual), to promote and facilitate new competences to spiritual and psychosocial professionals who are in crucial positions in communities and hospitals. Méthode The course was designed for priests, pastors, chaplains, social workers and psychologists from Ecuador involved in the care of patients with life-threatening illness, and it was conducted both in English and Spanish through a video conference platform, with live translation support. Specialists from both countries played key roles in this cooperation’s success. Résultats 21 participants from Ecuador attended the course: 1 doctor, 6 priests, 7 pastors, 1 psychologist, 1 social worker, 5 deacons and spiritual caregivers. Participants greatly valued the course content, the sharing of Swiss practices and the bilingual format. Upon completion, they received a signed certificate from Palliative.ch, the Swiss palliative care association. Conclusion The course focused on the assessment and management of symptoms associated with life-threatening illnesses and the dying process. After the course they were ready to approach medical teams to implement the spiritual and psychosocial dimension of Palliative Care and work with them towards setting up Palliative Care teams. The course also highlighted the essential role of the participants in providing spiritual and psychosocial care and support for the patients, their families and caregivers within the growing interprofessional palliative care teams, which improve the quality of care.


|
||
|
14:15 – 15:15
|
Séminaire parallèle 6 |
|
|
Salle d'atelier 5
Séminaire
|
Lisa Hentsch, Genève
|
|
|
FM21
Intégration structurée des soins spirituels en gériatrie aiguë : un projet pilote interprofessionnel
Yolanda Espolio Desbaillet, La Chaux-de Fonds
Abstract
Contexte
La prise en charge de la dimension spirituelle, constitutive de l’être humain, est un élément fondamental des soins palliatifs (Bigorio, 2008). L’unité des soins palliatifs du Réseau hospitalier neuchâtelois (RHNe) applique ces recommandations de longue date. Leur intégration reste à consolider dans la prise en charge palliative des patients d’autres unités. Nous supposons qu’une meilleure intégration des soins spirituels (SSpir) au sein des équipes soignantes interprofessionnelles améliore la prise en soins globale des patients. Objectiv Ce projet pilote interprofessionnel vise à explorer comment une formation de sensibilisation aux soins spirituels (ForSpir), combinée à une collaboration structurée avec l’aumônerie, peut améliorer la qualité des SSpir au sein de l’Unité de Gériatrie Aiguë (UGA) du RHNe, qui accueille des patients pouvant bénéficiant de soins palliatifs gériatriques. Méthode Une étude quantitative de type interventionnel pré-post, en deux phases, a été menée. Le Spiritual Care Practice Questionnaire (Parties I et II), administré avant et après une ForSpir donnée à l’équipe soignante de l’UGA, permet d’évaluer à la fois la manière dont les soignants perçoivent les SSpir et les barrières à leur mise en pratique. La phase 1 a débuté en juin 2023 avec l’administration pré du questionnaire suivi de la ForSpir. En janvier 2024, un système de coordination structuré avec les accompagnantes spirituelles (AS) a été mis en place, incluant des accompagnements personnalisés de patients, des transmissions orales et écrites, ainsi qu’un colloque hebdomadaire avec les médecins-assistants. La phase 2 du projet (administration post du questionnaire) est prévue à l’été 2025 pour évaluer les pratiques à 24 mois. Résultats Les résultats de la phase 1 (N=18) montrent que 82% des soignants considèrent que répondre aux besoins spirituels relève de leur rôle professionnel. Toutefois, 78% signalent un besoin de formation, 82% manquent de temps et 58% évoquent une difficulté à distinguer les SSpir du prosélytisme. Après 16 mois, les bilans du comité de pilotage confirment la pertinence de la collaboration avec les AS et l’engagement renforcé des équipes dans les SSpir. Conclusion Ce projet illustre la possibilité d’un modèle d’intégration interprofessionnelle applicable dans une unité de soins gériatriques. Les résultats préliminaires, à confirmer par la phase 2, indiquent que le langage commun entre soignants et AS, soutenu par des outils concrets, facilite l’identification précoce des besoins spirituels. |
||
|
FM22
Symptom burden, psycho-social & spiritual needs in Heart Failure: Swiss results from RAPHAEL
Catarina Letras, Lausanne
Abstract
Contexte
Despite growing recognition of palliative care (PC) in chronic diseases, there remains a significant knowledge gap in how to best integrate PC into the care of patients with heart failure (HF). These patients often live with burdensome symptoms and progressive limitations that affect their autonomy, identity, and relationships. Furthermore, the psychosocial and existential aspects of their care remain unexplored. Objectiv This study, part of the HORIZON Europe-funded RAPHAEL project, explores both the symptom burden and unmet social and existential needs among Swiss patients with HF living at home, as well as the perspectives of their informal caregivers. It aims to identify critical gaps in current support systems to guide better integration of PC across HF care pathways in Switzerland and Europe. Méthode A multiple method study is being conducted, targeting 10–15 HF patient–caregiver dyads. Adult patients diagnosed with HF and receiving home-based care, are being recruited through the hospital’s HF department. Patient symptom burden is being collected through the Utrecht Symptom Diary-4 Dimension (USD-4D), whilst patients’ and caregivers’ psychosocial and spiritual needs are being explored through semi-structured interviews. Descriptive statistics are used to describe symptom burden, whilst interviews are analyzed thematically using Braun & Clarke’s model, in combination with the QUAGOL method and the support of NVivo software. Résultats While data collection and analysis are ongoing, we anticipate emerging themes related to loss of independence, difficulty navigating care decisions, emotional fatigue among caregivers, and the need for earlier, individualized communication about future care options. These findings will contribute to both national and European-level insights into PC needs in HF contexts. Conclusion This study addresses a key gap in Swiss and European HF care by examining patient and caregiver experiences and patient’s symptom burden. This part of the project will contribute to provide evidence to inform healthcare delivery, workforce development, and public policy aimed at improving the quality and accessibility of integrated PC for people living with HF. |
||
|
FM23
« Je fais tout pour ne pas rentrer » : la complexité des discussions autour du retour à domicile en soins palliatifs.
Zaria Gossin, Lausanne
AbstractContexte Objectif Méthodes Résultats Discussion |
||
|
FM24
High-quality palliative care: a novel organisational management to support interprofessional paradigm
Tanja Fusi-Schmidhauser, Lugano
Abstract
Contexte
Specialised palliative care (PC) is defined by structured interprofessional work and collaborative work is a fundamental value for high-quality PC provision, since it offers a better perspective on patients’ needs. Nonetheless, PC institutions are not defining structures and processes for this area. Objectiv To illustrate the governance changes implemented by a specialised PC institution for the development of interprofessionality as a transversal model of care.
Méthode The board of directors (BoD) of the PC institution addressed the topic from a change management perspective, while considering that the institution itself guarantees the interprofessional governance. Therefore, a specific interprofessional area was established and a dedicated manager for this area was appointed, while joining the medical and nursing director of the PC institution within BoD. The manager of the interprofessional area plans, coordinates and monitors the specific activities in agreement with the medical and nursing area to obtain a systemic perspective within the institution. Résultats The establishment of an area dedicated to the topic of interprofessional and transdisciplinary work has created virtuous synergies within and outside the institution. Patients identify this righteous collaboration as better care and greater trust in the care providing teams. Furthermore, it helped to promote the analysis and comparison of clinical processes performed in different in-hospital specialties (cardiology, nephrology, neurology, among others), with attention to shared advance care planning. At last, the collaborative culture model was exported externally, allowing a better patient self-determination. Conclusion In regards to interprofessionality, the management of a specialised PC institution is the first driver of a cultural change through clear choices and a long-term commitment. Even in healthcare systems with critical financial issues, this choice promotes the development of opportunities instead of constraints, improves sustainability of care, saves costs, optimizes human resources and finally reduces the stress of healthcare professionals and thus turnover. |
||
|
14:15 – 15:15
|
Séminaire parallèle 7 |
|
|
Salle des sociétés
Séminaire
|
Caroline Hertler, Zürich
|
|
|
FM25
“I wish I knew”: Assessing perceived and actual knowledge of partners’ end-of- life preferences
Clément Meier, Lausanne
Abstract
Contexte
Despite the importance of surrogate decision-making by partners at the end of life, there is only limited research on older adults' knowledge of their partners' end-of-life preferences. Objectiv Hence, this study investigates older adults’ perceived and actual knowledge of their partners' preferences for end-of-life care and medical treatments. Méthode We analyzed data from 667 respondents aged 50+ from Wave 8 (2019/2020) of the Survey on Health, Ageing, and Retirement in Europe in Switzerland. We assessed respondents’ actual knowledge by comparing their perceptions of their partners' preferences forend-of-life care and medical treatments with the partners' self-reported preferences. Additionally, respondents were asked to rate their perceived knowledge of their partners' wishes. Associations were assessed using multivariable regression models, adjusting for social, health, and regional characteristics. Résultats Respondents' actual knowledge of their partners' preferences varied, with the share of correct answers ranging from 35% to 81% depending on the preferences. More than 80% of respondents felt that they knew their partners’ end-of-life and medical treatment preferences “rather” or “very” well, and those respondents were more likely to identify their partners’ preferences accurately. Conclusion Improved communication between partners regarding their end-of-life preferences could significantly enhance surrogate end-of-life decision-making. However, since older adults’ perceived knowledge of their partners’ preferences seems overly optimistic, they may see little need to initiate such conversations by themselves, emphasizing the need for external educational interventions such as role-plays or case study discussions through, say, the community, or healthcare system to encourage such conversations. |
||
|
FM26
“Thank you and keep it up”: a cross-sectional survey on care satisfaction in palliative care units
Tanja Fusi-Schmidhauser, Lugano
AbstractHintergrund Quality of care and satisfaction with care are two essential elements of palliative care (PC) provision. Satisfaction with care evaluates the fulfilment of expectations and needs of patients and their informal carers on provided PC in a specific healthcare setting. Evidence-based measures to define satisfaction and therefore quality of care are deemed necessary for the development of sustainable PC services. Despite this, data on satisfaction with care in specialised PC units are scarce. Ziel To explore satisfaction with care of patients and their families in specialised PC units. Methode A cross-sectional survey study conducted from December 4, 2023 to August 31, 2024 in two specialised PC units. Demographics and data on satisfaction with care were collected through a duly developed anonymized questionnaire for patients and informal carers. Written and electronic options through Q-Code were sent for compilation. The quality service of the department received the filled-out questionnaires and provided the raw data. Descriptive statistics supported data analysis. Resultate A total of 510 questionnaires (195 for discharged patients and their informal carers and 120 for bereaved families) were sent, 216 (42%) were returned to the quality service. The majority of respondents were patients (n=101) and bereaved family members (n=81). Patients reported a good relationship with the interdisciplinary team (physicians, nurses and allied healthcare professionals) and their needs were met as expected during hospitalisation. Bereaved families confirmed the attentive and personalised care and highlighted the important support they received by the interdisciplinary team during end-of-life care. Schlussfolgerung Key elements of PC provision, such as interdisciplinary work and personalised care increase patients’ and informal carers’ perception of satisfaction in specialised PC units. The sustainability of high-quality PC delivery should be driven by continuous monitoring of care satisfaction through a virtuous flow of feedbacks and revisions of all institutional processes. |
||
|
FM27
Challenges of the use of drugs for palliative sedation in dying residents in Swiss nursing homes
Maya Monteverde, Gümligen
Abstract
Hintergrund
At the end of life, patients frequently experience distressing symptoms. When they become refractory, medications for palliative sedation are used to alleviate unbearable suffering. Applying palliative sedation relies on defined procedures according to guidelines and should therefore be primarily conducted in specialist settings. However, little is known about how registered nurses (RN), advanced practice nurses (APN), and healthcare assistants (HCA) manage refractory symptoms in nursing homes, and how sedating medications for palliative sedation are used in this non-specialist setting. Ziel The aim of this study is to examine how RN, APN and HCA alleviate distressing and refractory symptoms in Swiss nursing homes, the challenges they face, the strategies and interventions they employ to alleviate residents’ suffering. Methode This qualitative study involved nursing personnel from seven nursing homes in German-speaking Switzerland. Until data saturation, seven semi-structured focus group interviews were conducted between October 2023 and January 2024, transcribed verbatim, and analysed using a grounded theory approach. Resultate Twenty RN, two APN and six HCA participated in the seven focus group interviews. A core category, ‘Tension between alleviating suffering and over-sedating’, was identified with three subcategories: (1) recognising suffering, (2) assessing suffering, and (3) alleviating suffering. Challenges included (a) distinguishing between own (healthcare professionals) and others’ (residents or relatives) suffering, (b) interactions with residents’ relatives and general practitioners (GP), and (c) uncertainties with sedating medication. Strategies they employed to address these challenges, such as (a) ‘double-checking principle’, (b) ‘getting everyone on the same page’, and (c) ‘safety net’, were identified. Personnel and financial resources, as well as individual beliefs and societal attitudes influenced the use of sedating medication. Schlussfolgerung RN, APN and HCA in nursing homes face complex challenges related to the use of sedating medication. Strategies such as emphasising shared decision-making, interprofessional collaboration and involving palliative care specialists are essential. Without applying these strategies, there is a risk to manage care demands rather than alleviate suffering appropriately by using sedating medication.
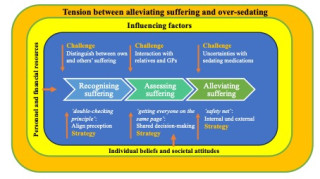
|
||
|
FM28
Erkenntnisse zu Geschlechtsunterschieden bei pflegenden Angehörigen von Menschen mit Demenz
Annemarie Schumacher Dimech, Luzern
AbstractHintergrund Angesichts der demografischen Alterung der Bevölkerung und der weltweit steigenden Inzidenz von Demenzerkrankungen gewinnt die Auseinandersetzung mit den Erfahrungen pflegender Angehörigen zunehmend an Bedeutung. Geschlechterspezifische Unterschiede in der Betreuungssituation sind vielfach belegt, wobei ein zentraler Aspekt darin besteht, dass weibliche pflegende Angehörige im Vergleich zu männlicher Angehörigen signifikant höhere Werte wahrgenommenen Stresses berichten. Da Stress mit negativen gesundheitlichen Folgen assoziiert ist, ist es zentral, den Einfluss von Bewältigungsstrategien, persönlichen Ressourcen und Betreuungsbedingungen auf diese geschlechtsspezifischen Unterschiede in der Stresswahrnehmung zu analysieren. Ziel Ziel dieser Studie ist es, Erkenntnisse zu geschlechterspezifischen Unterschieden bei Betreuungspersonen in der Zentralschweiz zu erfassen. Durch die Analyse des Zusammenspiels zwischen Geschlecht und verschiedenen Einflussfaktoren sollen Impulse für vertiefende Analysen sowie für die Entwicklung individualisierter Unterstützungsangebote generiert werden. Methode Mittels einer fragebogengestützten Erhebung wurden Daten von 224 pflegenden Angehörigen von Menschen mit Demenz in der Zentralschweiz gesammelt. Der Fragebogen umfasste unter anderem Angaben zu persönlichen Ressourcen und Betreuungskontexten. Zusätzlich beantworteten die Teilnehmenden vier standardisierte Instrumente zur Erfassung von Stresswahrnehmung, Bewältigungsstrategien, Resilienz und Einsamkeit. Resultate Die Analyse zeigt, dass weibliche pflegende Angehörige tendenziell ein höheres Mass an wahrgenommenem Stress berichten als männliche. Darüber hinaus passen Frauen ihre Erwerbstätigkeit häufiger an oder geben diese auf, um ihre Rolle als pflegende Angehörige wahrzunehmen. Hinsichtlich der Stressbewältigung zeichnen sich geschlechtsspezifische Unterschiede ab: Männer neigen vermehrt zu vermeidenden und ablenkungsorientierten Bewältigungsstrategien, während Frauen häufiger emotionale Unterstützungsaufgaben übernehmen, etwa durch Gespräche, aktives Zuhören oder tröstendes Verhalten. Zudem nehmen Frauen signifikant häufiger Unterstützung durch Familie und Freundeskreis in Anspruch, wohingegen Männer tendenziell eher auf professionelle Pflegedienste zurückgreifen. Diskussion Diese Untersuchung liefert vertiefte Einblicke in die Betreuungskontexte, das Stresserleben, die Bewältigungsstrategien und die Nutzung persönlicher Ressourcen von pflegenden Angehörigen von Menschen mit Demenz. Die Ergebnisse unterstreichen die Notwendigkeit, geschlechtersensible Unterstützungsangebote zu entwickeln, die auf die unterschiedlichen Belastungsprofile und Bewältigungsmechanismen eingehen. Eine differenzierte Betrachtung der Geschlechterrollen im Pflegekontext kann zur gezielten Entlastung von betreuenden Angehörigen beitragen. Weitere Forschung ist erforderlich, um die komplexen Zusammenhänge zwischen Geschlecht, Stresswahrnehmung und Bewältigung zu vertiefen und die Versorgungsstrukturen entsprechend anzupassen. Schlussfolgerung Die vorliegenden Ergebnisse verdeutlichen signifikante geschlechterspezifische Unterschiede in zentralen Aspekten informeller Betreuung, insbesondere im Hinblick auf Stresswahrnehmung, Bewältigungsstrategien und den Umgang mit Unterstützungsressourcen. Diese Erkenntnisse unterstreichen die Wichtigkeit einer geschlechterdifferenzierten Betrachtung in Forschung, Praxis und gesundheitspolitischer Planung, um bedarfsgerechte und wirksame Entlastungsangebote für pflegende Angehörige zu gewährleisten. |
||
|
15:15 – 15:30
|
Temps de transition |
|
|
Break
|
||
|
15:30 – 16:15
|
Table ronde |
|
|
Salle de concert
Special Session
|
Steffen Eychmüller, Bern
|
|
Comment mourrons-nous à l’avenir ?
Anita Fetz, Basel ; Christine Clavien, Genève; Claudia Gamondi, Lausanne; Settimio Monteverde, Zürich ; Jürg Caspar Streuli, St. Gallen
|
||
|
16:15 – 16:45
|
Pause café |
|
|
Break
|
||
|
16:45 – 17:45
|
Conférence principale 3Défis financiers dans les soins palliatifs |
|
|
Salle de concert
Conférence principale
|
Petra Vayne-Bossert, Genève
|
|
Des changements majeurs
Sébastien Jotterand, Aubonne
|
||
Musique Spitex
Mirjam Toews, Basel
|
||
|
19:30 – 23:00
|
Soirée récréativeRestaurant Brasserie Rotonde
|
|
|
Break
|