Jeudi, 27 novembre 2025
|
08:00 – 09:00
|
Enregistrement |
|
|
Break
|
||
|
08:30 – 10:00
|
Assemblée des délégué(e)s palliative.ch |
|
|
Salle d'atelier 1+2
Assemblée des délégué(e)s
|
||
|
09:00 – 10:00
|
Teach the Teachers |
|
|
Salle des sociétés
Special Session
|
Steffen Eychmüller, Bern
|
|
Training in Palliative Care at Swiss Medical Schools – an update
Steffen Eychmüller, Bern ; Claudia Gamondi, Lausanne
|
||
Communication skills: an area of specific competency in Palliative Care?
Sibylle Felber, Bern; Steffen Eychmüller, Bern
|
||
Smarter healthcare: Top 5 – recommendations for Palliative Care; an e-learning tool
Sandra Eckstein, Basel
|
||
|
09:00 – 10:00
|
Young Researchers, les voix de demain |
|
|
Salle de concert
Special Session
|
Lisa Hentsch, Genève ; Caroline Hertler, Zürich
|
|
|
FM29
Understanding Patient Altruism in Palliative Care: A Multimethod Study
Mathieu Bernard, Lausanne
Abstract
Contexte
Traditionally, patients in palliative care are viewed as passive recipients of support, with limited emphasis on their autonomy or capacity for meaningful action. This study explores altruism as a potential source of psychological well-being in end-of-life care. Objectiv We investigated the relationship between altruism and psychosocial outcomes, how patients define altruism, its significance during the final phase of life, and its evolution over the life course. Méthode This multimethod observational study was conducted across Switzerland’s three linguistic regions, integrating quantitative assessments, and qualitative interviews. Validated tools measured prosocial behavior, self-transcendent values, depression, anxiety, quality of life, meaning in life, and perceived burden. A reflexive thematic analysis was used for qualitative data, within a constructivist framework. Résultats In the quantitative sample, 123 patients participated. The qualitative subsample included 32 patients. Prosocial behavior was negatively correlated with depression (r=-0.326, p=0.005), and positively associated with quality of life (r=0.222, p=0.039). Associations in the same direction were found for altruistic values (benevolence and universalism). Interviews revealed that altruism remains central to patients’ identities, tied to values like justice and solidarity. While their conception of altruism stayed stable, its expression shifted due to physical limitations. Patients described tension between helping others and maintaining self-care. A new form of altruism emerged: vanishing – making oneself invisible to avoid burdening others. Conclusion Altruism is important in palliative care, aligning with literature on high self-transcendent values in older adults and the dying. Altruism acts as a protective factor against psychological distress (depression) and is positively associated with quality of life. Despite illness, patients maintain an altruistic identity, but physical decline limits their ability to give, leading to feelings of uselessness. Participants adopt adaptation strategies to restore balance and meaning. |
||
|
FM30
Professional Perspective on the Importance of Advance Care Planning: A Single-Oncology Center Study
Eva SL Pedersen, Bern
Abstract
Hintergrund
Advance Care Planning (ACP) among patients with advanced cancer reduces stress and emergency admissions and relieves burden of family caregivers. With cancer being the leading cause of death in Switzerland among adults above 45 years, improving ACP affects patients and families by a better goal-concordant care. However, ACP is still not fully integrated into standard cancer care. Understanding experiences of ACP and priorities for improvements among healthcare providers is essential for optimizing its clinical integration. Ziel Examining the importance of and experiences with ACP and priorities for improving ACP among healthcare providers caring for patients with advance-stage cancer. Methode Cross-sectional survey among oncology healthcare providers as part of a framework of evaluating the Concurrent Care (CoCa) project. CoCa aims to improve care among patients with advance-stage cancer through implementation and optimization of routine ACP using a pragmatic structure. We adapted an existing questionnaire to assess knowledge, experience, and importance of implementing ACP, which includes four sections: 1) Demographics including experience with ACP; 2) Rating importance of certain questions of patients, e.g. “How long will I live?”; 3) Evaluating which aspects of ACP are working and 4) which aspects of ACP could be improved. The questionnaire link was sent via email to 250 physicians and nurses in April 2025 via department heads. We compare knowledge, experience, and importance by responders’ profession. Resultate The questionnaire was completed by 64 (response rate: 26%); 17 physicians and 47 nurses. Median age was 39 years and 76% were women. Participants rated questions related to health complications as most important to patients, with little difference by profession. Physicians regard themselves as more confident/ having sufficient information and skills to address ACP compared to nurses. However, both groups prioritize communication skills training in ACP. The level of pre-information of patients about content and process of ACP was considered as relatively low. Improving the ACP process through coordination and documentation was of highest priority. Schlussfolgerung This study provides detailed data on knowledge, experiences, and importance of improving ACP implementation from the healthcare providers’ perspective and form the basis for creating standardized pathways and suitable training measures to integrate ACP and improve electronic documentation. |
||
|
FM31
Prepared for goodbye? End-of-life preparedness and emotional suffering among patients and caregivers
Clément Meier, Lausanne
Abstract
Contexte
Preparing for the end of life is believed to help mitigate emotional suffering for both patients and their caregivers. However, empirical evidence on the emotional benefits of feeling prepared for death remains limited. Objectiv This study uses longitudinal data from the international iLIVE project to examine how perceived end-of-life preparedness is associated with emotional suffering among patients and their caregivers before and after death. Méthode Data from 1,041 patients and 496 caregivers across 11 countries (Argentina, Switzerland, Germany, Spain, United Kingdom, Iceland, Netherlands, Norway, New Zealand, Sweden, Slovenia), enrolled in a prospective cohort study from the iLIVE project (2020–2023), were analyzed. Participants were surveyed at baseline, one-month follow-up, and where possible after the patient's death. The association between end-of-life preparedness (ICECAP-SCM) and emotional suffering (ICECAP-SCM & HGRC) was examined using OLS regression models, adjusting for socio-demographic and health-related covariates. Résultats Feeling fully prepared was significantly associated with lower levels of emotional suffering for both patients and caregivers. Among patients, preparedness was linked to reduced emotional suffering at baseline (AME = -0.17, p < 0.01) and follow-up (AME = -0.21, p < 0.01). For caregivers, these associations were even more pronounced at baseline (AME = -0.59, p < 0.001), follow-up (AME = -0.59, p < 0.001), and after the patient’s death (AME = -0.41, p < 0.05). Conclusion Perceived preparedness for the end of life seems to play a key protective role in reducing emotional suffering for patients approaching death and their caregivers, both during the illness and after bereavement. These findings highlight the importance of encouraging end-of-life planning to support emotional well-being across the final phase of life and beyond. |
||
|
FM32
Clinicians’ use of emotions during palliative care consultations: a constructivist grounded theory.
Katrien Moens, Bern
Abstract
Contexte
Palliative care clinicians are frequently exposed to emotionally charged situations. While emotions are an intrinsic part of their interactions with patients and relatives, the role of clinicians’ own emotions has remained understudied. Objectiv We aimed to explore how palliative care clinicians use their emotions during end-of-life care consultations as part of the way they provide care. Méthode We conducted a qualitative study using individual interviews with palliative care clinicians from different countries and backgrounds. Countries were selected based on their ranking on the Quality of Death and Dying Index. Interviews continued until we reached theoretical sufficiency. Twenty-two palliative care clinicians from 10 countries, including Switzerland, participated: two psychologists, four social workers, five nurses, and 11 physicians. Fourteen were women. Participants had an average of 13 years of palliative care experience and were on average 45 years old. We analyzed the data using a social constructivist grounded theory approach. Résultats The process of deciding when and how to use emotions could be understood as a three-phase process which was prompted by a difficult end-of-life interaction (e.g. confrontations with the emotions of patients/ relatives, ethical dilemmas or conflicts,) that triggered a strong emotion. Subsequently, clinicians became aware of the specific emotion via its physiological and/ or psychological cues. Next, an evaluation of the appropriateness of sharing the emotion followed, in which barriers and facilitators (e.g. the self-perceived level of emotional skills, the feeling of safety in the team) interplayed, influencing the clinicians to, in a final phase, decide to disclose their emotions in a verbal and/ or non-verbal way. All phases of the process were interrelated by the joint value of sharing emotions to build connection, the core category of the theory. Conclusion Our findings can help clinicians in determining the appropriateness of showing their emotions in clinical practice. When met with self-awareness and reflection, these emotions can serve as a valuable resource for delivering patient- and relationship-centred palliative care. Future research should explore clinicians’ attitudes and training needs regarding emotions skills training more broadly. |
||
|
FM33
Structuration de la visite médico-infirmière : un projet innovant en soins palliatifs
Marion Broucke, Blonay
Abstract
Contexte
Dans une perspective de renforcement de la collaboration interprofessionnelle et d’amélioration de la qualité des soins, un projet innovant a été mené au sein de trois unités pilotes membres de la Fédération des hôpitaux vaudois (FHV), dont une en unité de soins palliatifs spécialisés. Objectiv Ce projet interinstitutionnel visait l’implantation de la trame SCAR (Situation, Contexte, Appréciation, Recommandation), outil structurant issu de TeamSTEPPS, pour encadrer la visite médico-infirmière et ainsi diminuer le risque d’erreurs, optimiser la planification des soins et l’expérience patient. Méthode Reposant sur une méthodologie rigoureuse d’implantation fondée sur les cadres théoriques I-PARISH et CFIR, le projet s’est articulé autour d’une gouvernance interinstitutionnelle, d’un accompagnement local au changement et d’une personnalisation des stratégies d’implantation à chaque unité. Les stratégies comprenaient notamment la diffusion de supports didactiques, la désignation de référents cliniques et l’élaboration de cartes-mémos pratiques. Résultats En soins palliatifs, cette démarche a permis d'améliorer la structure de la visite, la fluidité et la pertinence des échanges interdisciplinaires, tout en renforçant la centration sur les besoins réels des patients avec notamment l’intégration du concept « qu’est-ce qui est important pour vous ? ». La révision quotidienne et systématique de l’ensemble des traitements a permis une optimisation de la médication. Discussion La réalisation de vidéos servira de support formateur pour les nouveaux collaborateurs et éventuellement de modèle pour d’autres structures de soins palliatifs. Conclusion Ce projet illustre les bénéfices d’une démarche collaborative interétablissement et souligne l’intérêt de structurer les visites médico-infirmières dans des contextes complexes comme celui des soins palliatifs. Il offre une voie concrète vers une meilleure coordination des soins, dans le respect des valeurs humaines fondamentales de cette discipline. 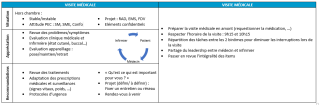
|
||
|
FM34
Palliative Care für Menschen mit kognitiver Beeinträchtigung – «über das Thema reden»
Sibylla Strolz, St. Gallen
Abstract
Hintergrund
Erhebungen in der Schweiz zeigen, dass die Zahl der Menschen mit kognitiven, körperlichen oder psychischen Beeinträchtigungen, welche 55 Jahre und älter werden, wächst. Damit einher geht die steigende Prävalenz chronischer & altersbedingter Erkrankungen sowie der zunehmende Bedarf an an Palliative und End-of-Life-Care. Damit sich Menschen mit kognitiven Beeinträchtigungen mit dem Thema Lebensende auseinandersetzen können, braucht es adaptierte Kommunikationsmittel. Es gibt zahlreiche Tools, die jedoch meist formularbasiert sind (z.B. Vorsorgeauftrag in Leichter Sprache). Es fehlt an flächendeckenden sprachlich und kulturell adaptierten Materialien. Ziel Das PAL_Link Forschungsprojekt zielt darauf ab, ein Palliative und End-of-Life Care-Versorgungskonzept für erwachsene Menschen mit kognitiver Beeinträchtigung in der Ostschweiz zu entwickeln. Ein Teilprojekt davon widmet sich der Thematik Kommunikation.
Methode Das PAL_LINK-Teilprojekt Kommunikation (2024–2025) schliesst Personen mit kognitiven Beeinträchtigungen partizipativ in den Entwicklungsprozess mit ein. Gemeinsam werden bestehende Tools geprüft und neue Zugänge erprobt und entwickelt. Resultate Aktuell sind zwei Elemente in Bearbeitung:
Schlussfolgerung Partizipative Herangehensweisen sind in Entwicklungsprojekten essentiell, damit sie an der Lebenswelt der betroffenen Personen anknüpfen und nachhaltig implementiert werden können. Am Kongress werden Erfahrungen mit den partizipativ erarbeiteten Kommunikationstools zusammen mit 1-2 Co-Forschenden geteilt. |
||
|
FM35
Deskriptive Analyse zur Nutzung eines Kinderhospizes in der Schweiz im ersten Betriebsjahr
Cathrine Liechti, Bern
Abstract
Hintergrund
In der Schweiz leben ca. 10’000 Kinder mit lebenslimitierenden Erkrankungen, deren Versorgung hohe Anforderungen an die betreuenden Familien sowie an das Gesundheitssystem stellt. Während Kinderhospize in mehreren europäischen Ländern ein etablierter Bestandteil der pädiatrischen Palliativversorgung sind, wurde in der Schweiz im August 2024 erstmals ein solches Angebot eröffnet. Das Kinderhospiz ergänzt die bestehende Versorgung durch spezialisierte Angebote wie Kurzzeitpflege, Brückenpflege und Betreuung in der End-of-Life-Phase. Ziel Ziel ist es, aufzuzeigen, wie das erste Kinderhospiz der Schweiz im ersten Betriebsjahr von betroffenen Familien genutzt wurde. Methode Es erfolgt eine deskriptive Analyse der Nutzer: innen (Kinder/ Familien) im Zeitraum von August 2024 bis Juli 2025. Erhoben werden demografische Merkmale (Alter der Kinder, Diagnosegruppen), familiäre Rahmenbedingungen (Anzahl Geschwisterkinder, Begleitpersonen), genutzte Angebote sowie Aufenthaltsdauer. Ergänzt wird die quantitative Datenerhebung durch qualitative Aussagen elterlicher Bezugspersonen und betroffener Kinder, welchen Nutzen ihnen das Kinderhospiz bringt. Resultate Zum Zeitpunkt der Einreichung liegen noch keine Ergebnisse vor. Die Datenerhebung läuft bis Juli 2025. Die Auswertung ist für August und September 2025 vorgesehen. Schlussfolgerung Die Resultate sollen aufzeigen, welchen konkreten Nutzen ein Kinderhospiz für betroffene Familien bietet und wie das Versorgungsangebot in Anspruch genommen wird. Die Erkenntnisse dienen als Grundlage für die Weiterentwicklung und strukturelle Verankerung von Kinderhospizangeboten in der Schweiz und sollen aufzeigen, welcher Bedarf an dieser Versorgungsform besteht. |
||
|
10:00 – 10:30
|
Pause café |
|
|
Break
|
||
|
10:30 – 10:45
|
Bienvenue |
|
|
Salle de concert
Special Session
|
||
|
par la conseillère fédérale
Elisabeth Baume-Schneider, Membre du Conseil fédéral
|
||
|
10:45 – 11:30
|
Conférence principale 4Autres pays, autres mœurs |
|
|
Salle de concert
Conférence principale
|
Monica Fliedner, Bern
|
|
Les soins palliatifs en Allemagne
Heiner Melching, Deutsche Gesellschaft für Palliativmedizin
|
||
Les soins palliatifs en France
Vianney Perrin, Morges
|
||
|
11:30 – 12:00
|
Remise des prix d’abstract palliative.ch |
|
|
Salle de concert
Special Session
|
David Blum, Zürich ; Manuela Weichelt, Präsidentin palliative.ch ; Lisa Hentsch, Genève
|
|
|
12:00 – 13:15
|
Buffet déjeuner & Présentation des posters |
|
|
Break
|
||
|
12:15 – 13:00
|
Réunion du groupe d’experts Aumônerie |
|
|
Salle des sociétés
Special Session
|
||
|
12:15 – 13:00
|
Réunion du groupe d’experts Soins infirmiers |
|
|
Salle de concert
Special Session
|
||
|
12:15 – 13:00
|
Réunion du groupe d’experts Médecins |
|
|
Salle d'atelier 1+2
Special Session
|
||
|
12:15 – 13:00
|
Versammlung der Fachgruppe Physiotherapie |
|
|
Salle d'atelier 5
Special Session
|
||
|
13:15 – 14:15
|
Séminaire parallèle 8 - spécifique aux soins |
|
|
Salle de concert
Séminaire
|
Claudia Schröter, Biel
|
|
|
Indikationskriterien für spezialisierte Palliative Care, ein Projekt der Deutschschweizer MPDs
Daniela Foos, Aarau; Michael Bruhin, Zürich
|
||
Therapeutic Touch – die Kunst der heilsamen Berührung
Josefine Hörburger, Wolfurt
|
||
|
13:15 – 14:15
|
Séminaire parallèle 9 - spécifique aux médecins |
|
|
Salle d'atelier 1+2
Séminaire
|
Fusi-Schmidhauser Tanja, Lugano; Sandra Eckstein, Basel
|
|
Closing the gender gap: transforming the future of palliative care research
Caroline Hertler, Zürich
|
||
Apomorphine infusions to improve the comfort of patients with advanced Parkisonian syndroms
Simon Singovski, Collonge-Bellerive
|
||
Ladies first? Gender differences in palliative care
Micaela Mare, Bellinzona
|
||
|
13:15 – 14:15
|
Séminaire parallèle 10 - spécifique pour les thérapies |
|
|
Salle d'atelier 5
Séminaire
|
Martina Egloff, Bern
|
|
Lymphtherapien in komplexen palliativen Situationen
René Heynen, Bern
|
||
L’hypnose, un langage commun au service de la personne en soins palliatifs
Petra Vayne-Bossert, Genève
|
||
|
13:15 – 14:15
|
Séminaire parallèle 11 - spécifique à l'aumônerie |
|
|
Salle des sociétés
Séminaire
|
Stefan Mayer, Aarau
|
|
|
Soins infirmiers – soins spirituels : travail interprofessionnel dans une équipe mobile de soins palliatifs
Anne-Sylvie Martin, Rennaz; Irene Stuby, Rennaz
|
||
Les soins palliatifs pédiatriques avec ou sans accompagnante spirituelle – une différence ?
Fabienne Christ, Lausanne ; Estelle Monnet, Lausanne
|
||
|
14:15 – 14:45
|
Pause café |
|
|
Break
|
||
|
14:45 – 15:45
|
Conférence principale 5Du début à la fin de la vie |
|
|
Salle de concert
Conférence principale
|
Ralf J. Jox, Lausanne
|
|
Intro
Ralf J. Jox, Lausanne
|
||
Aspects pédiatriques
Eva Bergsträsser, Zürich
|
||
Aspects gériatriques
Petra Vayne-Bossert, Genève
|
||
Aspects spirituels
Traugott Roser, Münster
|
||
|
15:45 – 15:50
|
Mot de clôture et fin du congrèsRétrospective et perspectives |
|
|
Salle de concert
Special Session
|
Corina Wirth, palliative.ch
|
|
|
15:50 – 16:20
|
Apéritif d'adieu |
|
|
Break
|